Research Area:
Responsible:
Research Lines:
Project abstract
Glioblastoma and skull base chordoma are among the most aggressive types of brain tumors, with an extremely poor prognosis. Most tumors recur within months after surgical and chemo-radiotherapy treatments.
Recurrence is driven by tumor heterogeneity, as different tumor regions with distinct biological properties respond differently to treatment. Tumor hypoxia (low oxygenation) is the primary cause of radiotherapy resistance in heterogeneous tumors and is linked to poor patient outcomes.
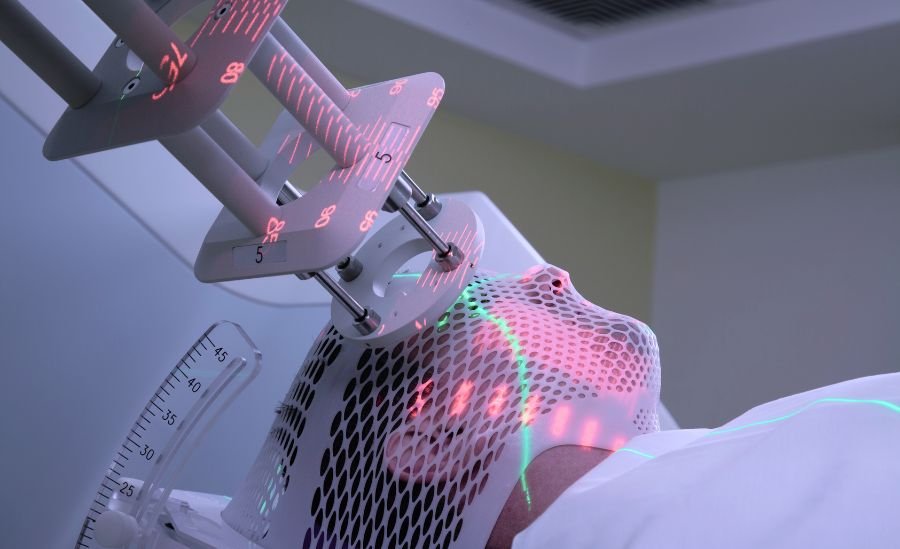
Effectively counteracting tumor hypoxia requires delivering higher radiation doses selectively to hypoxic tumor regions. This is challenging with conventional radiotherapy, which administers a uniform, moderate radiation dose to the entire tumor target. Strategies to increase the target dose are limited by established toxicity constraints to protect critical surrounding brain structures. Conventional radiotherapy plans do not incorporate tumor hypoxia measurements due to the limitations of current imaging techniques used for treatment planning.
The HYPERACT – Quantitative HYpoxia imaging for charged ParticlE Radiation treatment guidance: an improved strategy for Aggressive brain Cancers Treatment project aims to enhance radiotherapy for heterogeneous tumors by combining quantitative MRI/PET imaging—to non-invasively characterize hypoxic tumor regions—with carbon ion radiotherapy, which allows for the delivery of higher radiation doses to these regions while sparing the surrounding healthy tissue. This approach will enable a more effective radiation dose distribution, offering an opportunity to improve local tumor control, survival outcomes, and patients' quality of life.